Abstract
Introduction: Achievement of MRD negativity (MRD-) in MM is associated with superior progression free survival (PFS) and overall survival (OS). This is especially true after optimal induction followed by high-dose melphalan and autologous stem cell transplant (ASCT). Furthermore, lenalidomide (Len) maintenance following ASCT can further increase conversion to MRD- in patients (pts) that are MRD+ after ASCT. Daratumumab (Dara) has emerged as an extremely effective agent and Dara-containing regimens are associated with unprecedented MRD- rates. Still, the role of Dara in pts who are MRD+ to increase conversion to MRD- has not been studied. We report data from a phase 2 trial evaluating the efficacy of pre-ASCT Dara intensification and post-ASCT Dara maintenance in pts with MM, along with alternative Dara schedule to explore optimal frequency of administration for this immunotherapy approach.
Methods: This ongoing phase 2 trial (NCT03477539) enrolled pts with MRD+ (measured at 10-5 by multiparametric flow cytometry (MPF) in bone marrow) after any induction therapy prior to ASCT. Pts then received 2-4 (4 cycles allowed due to COVID pandemic and any ensuing delay in ASCT) 28d cycles of subcutaneous Dara 1800mcg pre-ASCT followed by ASCT, and maintenance starting at day-100 post-ASCT. Maintenance therapy included monthly Dara with Len (10mg 21 days on, 7 days off) for 1 year, and then single-agent Dara every 3 months until disease progression. MRD assessment on trial was done pre-ASCT, on Day-100, and at the end of 1-year Dara-Len maintenance therapy. Key eligibility criteria included: Induction therapy for pathologically confirmed MM, MRD+, adequate marrow (absolute neutrophil count ≥1.0x109, platelets ≥50x109) and organ function (creatinine clearance ≥30 mL/min), and ECOG performance status ≤2. Primary objective was MRD- rate at day-100 post-ASCT. The trial utilized a two-stage Simon optimum design to test the null hypothesis of MRD- rate at day-100 being 45%.
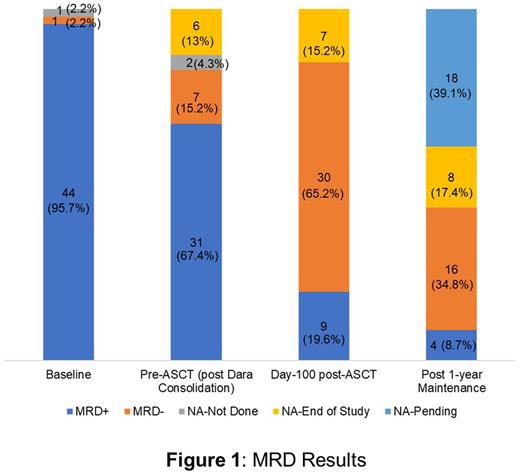
Results: Of the 50-pts enrolled, 46 were evaluable for primary endpoint analysis (3 were ineligible and 1 withdrew consent prior to the start of treatment). Median follow-up was 18.1 mths. The median age was 64 years (range: 44-73), with 8 (17.4%) pts having ISS III disease at enrollment. Seven (15.2%) had high-risk cytogenetics; del17p in 2 (4.3%), t(4;14) in 4 (8.7%), and t(14;16) in 2 (4.3%). Most common induction regimens were bortezomib+len+dex (VRd; 71.7%), Carfilzomib+Rd (KRd; 8.7%), Cyclophosphamide+Vd (VCd; 4.3%), Vd (4.3%), and Rd (4.3%). 38 (82.6%) pts were enrolled after initial induction for MM and 8 (17.4%) pts had second-line induction prior to study enrollment. Pre-ASCT Dara treatment included 2 cycles in 37 pts (80.4%) and 4 cycles in 9 pts (19.6%). At the pre-ASCT testing (after Dara treatment), 7 pts had converted to MRD- (6 of the pts with 2 cycles of Dara and 1 with 4 cycles of Dara). At Day-100 post-ASCT, 30 (65.2%; 95% CI: 50.5%-77.9%) of 46 pts were MRD-, 22 pts (47.8%) who were MRD+ after 1-4 cycles of pre-ASCT Dara consolidation, became MRD- at Day-100 (Figure 1). Twenty pts (of the 46) have been evaluated for MRD after 1 year of Dara-Len maintenance; 14 (30.4%) remained MRD-, 2 (4.3%) converted to MRD- after being MRD+ at Day-100, 3 (6.5%) remained MRD+, and 1 (2.2%) converted MRD+ after being MRD- at Day-100. Forty-nine pts received at least one cycle of treatment and were evaluable for adverse event (AE) analysis. The most common treatment related grade 3/4 AEs were neutropenia (69.4%), thrombocytopenia (69.4%) and leukopenia (57.1%).
Conclusion: Treatment regimens leading to MRD- state are preferred but so far MRD- cannot be guaranteed when selecting induction regimens. Pre-ASCT Dara consolidation followed by post-ASCT Dara-based maintenance in MM pts after induction therapy is a safe and effective strategy to enhance achievement of MRD- state. We also noted an alternative Dara regimen with extended treatment interval and continued efficacy. These early findings support continued investigation of Dara-based therapy as pre-ASCT intensification and post-ASCT maintenance to achieve deep responses, especially where induction therapy fails to achieve MRD- state.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal